I’ve been integrating yoga into my pelvic floor physical therapy practice since 2007.
Why?
Because yoga is a useful strategy for people to use at home to decrease pelvic pain and maintain the gains they experience during the rehab process. Having a home yoga program can reduce the intensity and frequency of flare-ups.
How? Yoga:
- supports the nervous system
- retrains the brain that movement can be pain-free
- increases flexibility of muscles and pliability of myofascial tissue
- increases awareness of your body
- pairs well with mindful breathing
- encourages you to be present and kind to yourself
Yoga supports the nervous system
When we experience real or perceived danger, the fight, flight, freeze response (sympathetic nervous system) will kick into action, preparing the body to escape from the situation if needed. Read about the connection between pelvic pain and the nervous system.
We want to increase the activity of the parasympathetic nervous system (“rest and digest”) so the heart rate, blood pressure, and respiratory rate all decreases. Sometimes we also see a decrease in pain, anxiety, and catastrophizing when the parasympathetic nervous system is active.
Yoga is a fabulous tool to increase the activity of the parasympathetic nervous system. Gentle yoga postures, meditation, mindfulness, and pranayama are all aspects of a yoga practice that can be very supportive for people with pelvic pain.
Yoga retrains the brain
When we experience persistent pelvic pain, our brain adapts to expect that area of our body to be in danger. The heightened sympathetic nervous system response becomes the default.
With a mindful gentle yoga practice, we can discover what movements are pain-free and change the expectation that movement will result in pain.
In doing so, we reprogram the brain to change the imprint that movement is dangerous or will be painful. We don’t further sensitize unconscious brain to expect movement to hurt.
Understanding that the pain signal originates in the brain, we can use that same brain to retrain what the expected outcome should be.
In the clinic, we retrain pelvic floor muscle overactivity (also referred to as pelvic floor muscle spasm) with manual therapy.
We utilize techniques like gentle myofascial release and other soft tissue mobilizations to encourage softening and elongation of the pelvic floor. After receiving myofascial release, visceral mobilization, or other connective tissue mobilization, you’ll have a new range of motion.
When you keep moving in your new range of movement, you not only maintain mobility, you remind your body it is safe to move.
You can augment treatment you receive at the clinic and continue retraining your brain by performing movement at home that is pain-free and supportive to the nervous system.
This is where yoga comes in. Through gentle yoga postures, you maintain your mobility and retrain your brain that movement doesn’t have to be painful.
Yoga is a valuable tool for retraining the brain but that’s not the only tool in the toolbox.
What makes you happy? Walking, dancing in your living room, or gardening all encompass movements that encourage mobility.
In addition to yoga postures targeted to relieve pelvic pain, the use of pranayama, or breath work, is particularly helpful in retraining the brain. Conscious breathwork restores the balance of the autonomic nervous system by decreasing the fight or flight response.
Yoga increases flexibility
What do you think of when you see the word flexibility? Do you think muscles? You’re right, but that’s not all yoga does in terms of flexibility.
In fact, yoga increases the pliability of connective tissue and flexibility of the myofascial attachments to the pelvis.
Fascia is the tissue that surrounds muscles, nerves, organs, etc. It’s the glue that keeps our body together. We can think beyond the muscles becoming more flexible and imagine the fascia surrounding the organs and nerves releasing as we rest and breath in a posture.
Yoga can provide the opportunity to increase flexibility of the muscles and decrease fascial stiffness. Decreased fascial stiffness around the nerves allow them to have the space they need to slide and glide without getting irritated.
For example, let’s imagine I am suffering from constipation. Constipation can be caused by many things: pelvic floor incoordination, pelvic floor tightness, slow gut motility (contractions called peristalsis), diet, hydration, or abdominal/pelvic adhesions.
Let’s say my constipation is caused by abdominal adhesions. Picture adhesions as the fascia between the organs creating little bridges between the organs and what was once two organs sliding next to each other becomes more “stuck.”
I might find twist postures (Supine Twist is one example) to be helpful. Twists offer a lengthening of the trunk and hip muscles.
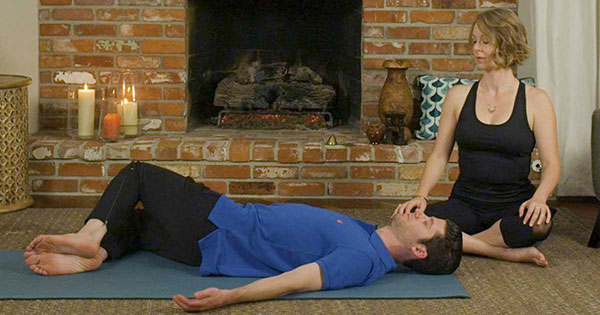
Supine Twist can be helpful in easing fascial stiffness around abdominal organs caused by constipation.
Conscious breath (think of breathing into the belly and the ribs) may even help release the deepest restrictions.
Our entire body is all connected. If I experience persistent coccydynia (tailbone pain), I will probably have restrictions above and below the epicenter of pain.
Yoga postures encourage mobility along an entire restricted plane, rather than just stretching one muscle (e.g. targeting the superficial back line with Downward Facing Dog).

Downward Facing Dog allows you to increase mobility along your entire back plane.
My final thoughts on flexibility: very often we are taught we need to stretch to become more flexible. Sometimes we might find more success resting into a posture, especially if we experience hypermobilility.
Yoga increases awareness
People who experience persistent pain might disassociate from the body part that is causing pain.
Grounding yoga practices helps renew one’s relationship with their physical body. Grounding techniques decrease dissociation and anxiety.
Two easy postures to practice at home are Seated and Standing Mountain Pose.
When practicing Seated Mountain, feel your sitz bones heavy into the chair while imagining a string lifts up your spine and through the top of your head.

Seated Mountain pose
When practicing Mountain Pose in standing, feel your feet grounding down magnetically into the earth.

Mountain pose
Yoga doesn’t just help integrate the mind and body, it integrates the spirit as well. Recognizing and allowing the flow of emotional response can very therapeutic as sometimes emotions can get stuck in the physical body.
Having strategies like yoga, breathwork, and mindfulness practices helps set you up for success during flare-ups!
Yoga and breathing (pranayama) are a perfect pairing
Every time we take a breath, we mobilize our pelvic floor muscles. When we inhale, the diaphragm and pelvic floor both descend towards our feet.
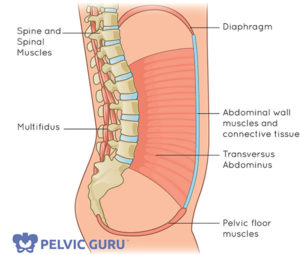
When we breath, both the diaphragm at the top and the pelvic floor descend. Illustration courtesy of Pelvic Guru
Pranayama, or breath work, supports the biomechanics between the pelvic floor muscles and the diaphragm. We can use this breath visualization to enhance this relationship and improve coordination. (A much better alternative to being told “you just need to relax!”)
Because of the direct mechanical relationship between the diaphragm and the pelvic floor, holding the breath can lead to pelvic floor muscle holding.
Sometimes we may not be aware we are holding our breath because of pain or even in anticipation of pain. By building awareness, which is a learned skill, we begin to notice and eventually control non-optimal breathing patterns.
Integrating breath with gentle movement has proven to be highly beneficial for people with persistent pelvic pain. Simple belly breathing lowers heart rate, blood pressure, and anxiety levels.
Yoga encourages being present and kind to yourself
Negotiating medical system can leave people feeling traumatized. Sadly, the percentage of folks who have experienced additional traumas (ie: verbal, physical, sexual, emotional etc.) are quite high.
Training the mind-body-spirit connection helps us to stay in the present moment rather than think about past painful experiences or anticipate future expectations of pain.
Encourage yourself to move at your own pace and comfort level. Find a gentle, loving acceptance of yourself and where you are in your healing journey.
Clinicians must be mindful to avoid any potential trauma triggers (i.e. teaching Bound Angle in an open gym area). An excellent book to read on this subject is Overcoming Trauma through Yoga by Emerson and Hopper.
Takeaways
Don’t lose hope! Some people have found a way to help reduce their suffering with mindful movement, meditation, breathwork, and yoga in addition to traditional medical approaches.
Recommended readings and videos
- How to use presence to work with pain, adapted from a Tara Brach workshop I attended
- “8 Strategies to Relieve Pelvic Pain” (Your Pace Yoga blog)
- Tame the Beast (video and website)
- “Why Things Hurt” TEDx talk by Lorimer Moseley
